Artificial intelligence and emerging technologies are transforming healthcare. From robotic surgery to early cancer detection algorithms, innovations are rapidly changing medical practice. This acceleration demands new approaches to medical education so graduates are prepared to utilize these tools safely, effectively, and ethically. Medical schools must rethink curricula, teaching methods, and learning environments to equip students for the AI-enabled clinical environments ahead.
Understanding AI and Its Impact
Artificial intelligence (AI) refers to computer systems that can perform tasks normally requiring human intelligence, such as visual perception, speech recognition, and decision-making. Machine learning, a type of AI, allows systems to learn from data without explicit programming. Deep learning uses multi-layered neural networks modeled on the brain’s structure.
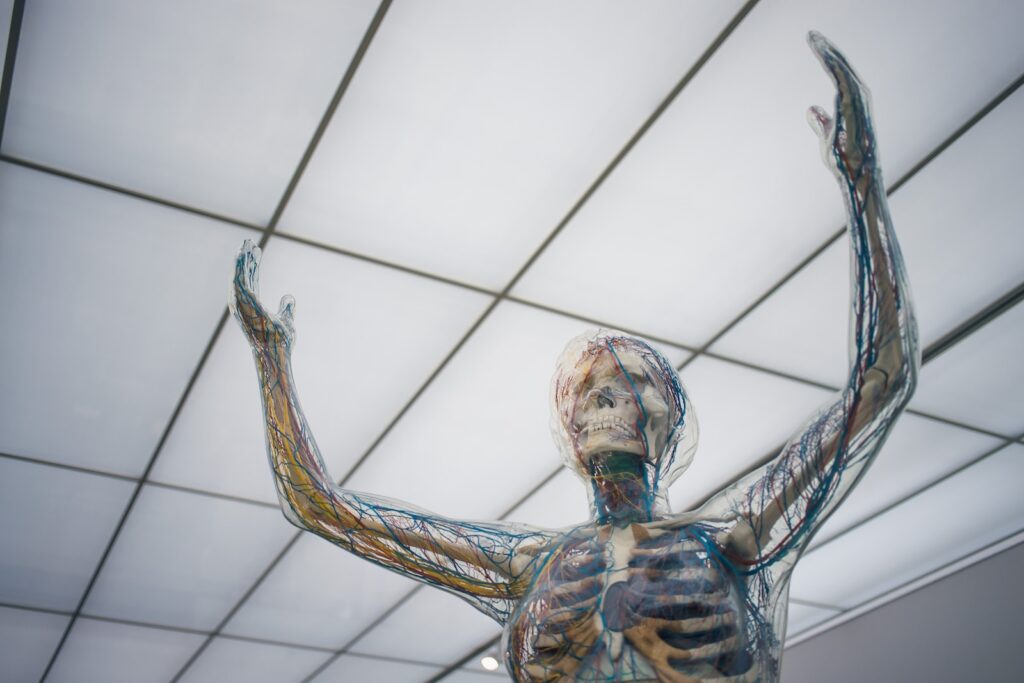
These technologies are powering innovations across healthcare. AI systems can analyze complex medical data to identify disease risk factors or early warnings. Machine learning algorithms can integrate and interpret imaging, lab tests, and clinical notes to make diagnostic suggestions. AI chatbots act as virtual health assistants. Surgical robots utilize computer vision and precision control beyond human capability.
However, AI has key limitations in healthcare. Algorithms rely heavily on training data quality and can perpetuate biases. They cannot yet replicate clinical judgement and human connections vital for care. Physicians will always play central roles in integrating AI insights and leading care teams.
Overall, though, AI will profoundly alter clinical practice. A survey of healthcare leaders found that 85% expect AI to revolutionize medicine in the next decade. Medical schools must take action now to prepare students or risk graduating clinicians unready to practice modern healthcare.
Rethinking the Core Medical Curriculum
Integrating AI appropriately into the curriculum begins with building students’ foundational competencies. Traditional basic science teaching emphasizing rote memorization remains essential for developing clinical reasoning. However, coursework must also provide a deeper conceptual understanding of human health and disease processes.
With this strengthened foundation, students can better evaluate AI technologies’ clinical value and limitations. Core courses should include primers on AI approaches relevant for medicine like neural networks, computer vision, natural language processing, and statistical learning. A basic understanding of how these methods work and potential biases informs appropriate clinical application.
The shifted curriculum must balance biomedical and digital literacy. Students still need robust anatomy, physiology, pathology, and related knowledge. But paired with introductions to data science and AI, this equips them to navigate both the capabilities and constraints of technologies they will utilize daily.
Learning by Doing: AI in Clinical Environments
Lectures on AI principles are only the beginning. The central curriculum transformation requires integrating AI technologies into clinical learning environments. Medical schools should partner with health systems to provide exposure to real-world implementation of AI-enabled diagnosis, monitoring, treatment planning, and interventions.
For instance, students could train diagnostic algorithms with proper data curation techniques. They could shadow physicians collaborating with AI chatbots gathering patient histories. Rotations could include observing robotic surgery and computer-aided medical procedures.
Hands-on experience develops understanding of clinical workflows integrating AI assistance. Students witness challenges that arise, such as discrepancies between algorithmic recommendations and physician judgement. They gain crucial skills for maximizing technologies’ benefits while recognizing their constraints and biases.
Rethinking Pedagogical Approaches
These curricular shifts necessitate evolving educational approaches. Passive lecturing cannot adequately prepare students for dynamic AI-powered clinical environments. Interactive methods like team-based learning, hackathons, and design projects better build needed skills.
Design thinking challenges students to develop AI solutions addressing real clinical problems. Hackathons encourage quickly prototyping and testing ideas, promoting computational creativity. Discussion cases can highlight ethical dilemmas introduced by AI, such as accountability gaps or biases.
Active pedagogies teach students to collaboratively and iteratively solve complex problems just as innovating with AI requires. This fosters the adaptability and critical thinking vital for safely adopting emerging technologies while providing outstanding patient care.
Developing a New Generation of Clinician-Innovators
To fully prepare students, medical schools should nurture the next generation of physician-innovators who can advance healthcare AI themselves. New tracks, concentrations, and institutes should cultivate those pursuing this career path.
For interested students, foundational AI/data science coursework can be expanded into hands-on research assisting faculty projects. Electives can dive deeper into medical AI/machine learning methods and their clinical translation. Business/entrepreneurship offerings can teach skills for taking discoveries from bench to bedside.
With this specialized training, some graduates will become clinician-scientists leading cutting-edge research at academic medical centers. Others may join startups or tech companies as physician consultants ensuring technologies meet patient needs. Still more may bring innovative thinking to healthcare organizations as CMIOs.
Schools should showcase these alumni role models and provide networking opportunities with them. Mentorship from physician-innovators demonstrates exciting possibilities at the intersection of medicine and technology.
Reimagining Learning Spaces
Integrating AI into health professions education also requires reimagining physical learning spaces. Classrooms must flexibly support varied active learning methods and peer interaction. Movable furniture facilitates reconfiguring layouts for team projects. Videoconferencing and interactive displays enable collaboration.
Maker spaces provide access to technologies like 3D printers and electronics. Simulation centers mimic clinical environments with intelligent mannequins and virtual reality. Insights labs house computing power, data visualization tools, and devices to investigate healthcare AI. Modern spaces like these foster the critical thinking and creativity fueling innovation.
The Future of Medical Education: Adapting to Changing Roles and Responsibilities
Medical education is undergoing significant changes as the world evolves and new technologies emerge. In a recent lecture at the Virginia Tech Carilion School of Medicine, renowned medical education expert Dr. Ronald Harden predicted that the roles of teachers and students will adapt, with students becoming more involved as partners in developing their educational programs. This shift reflects the need for medical schools to keep pace with our rapidly advancing knowledge base and prepare students for lifelong learning and careers we can’t yet imagine.
The Changing Landscape of Medical Education
Several factors are driving the transformation in medical education that Dr. Harden describes. First, the COVID-19 pandemic demonstrated the importance of independent learning skills. With lockdowns and social distancing policies, traditional classroom teaching was disrupted globally. Students who could take charge of their own education fared better in this unprecedented situation. Self-directed learning skills will only grow more vital as medical students prepare for a career in which knowledge evolves swiftly.
Additionally, artificial intelligence and other new technologies are revolutionizing healthcare. The practice of medicine in 20 years may look very different than it does today. Medical students must learn to adapt and take advantage of cutting-edge developments in order to provide the best possible care throughout their careers. An education focused solely on current knowledge will not suffice.
Finally, the sheer pace of advancement in the medical sciences is rapidly accelerating. The doubling time of medical knowledge continues to decline. It’s estimated that by 2020, medical knowledge was doubling every 73 days. Even accounting for future slowing, this exponential growth makes it impossible for students to master static sets of facts. Education must equip them for lifelong learning to stay updated in their specialties.
Adapting Teacher and Student Roles
To address these changing dynamics, Dr. Harden advocates reimagining the roles of teachers and students. The days of teachers as pure content experts and students as passive recipients of knowledge are over.
Rather than transmitters of information, Dr. Harden sees teachers becoming guides, mentors, and facilitators. They will work with students to help shape their educational journeys based on their skills, interests, and goals. Curricula will become more personalized, moving away from the “one size fits all” model.
Students will take a much more active role as partners directing their learning. They will identify knowledge and skill gaps and choose educational experiences accordingly, with input from faculty mentors. Students may also participate in developing innovative curricular components that address emerging topics or new technologies.
This partnership model aligns with adult learning principles. It engages students’ intrinsic motivations to learn what they need to succeed in their chosen specialties. They assume personal responsibility for the lifelong self-directed learning their future careers will require.
Advantages of Smaller Schools
These curriculum changes may prove easier to implement at smaller institutions like the Virginia Tech Carilion School of Medicine (VTCSOM). With around 400 students across four class years, VTCSOM provides opportunities for personalized education within a collaborative learning community.
For instance, VTCSOM utilizes problem-based learning. Students work together in small groups to solve open-ended real world cases. This approach develops clinical reasoning and self-directed learning skills applicable throughout their careers. Smaller class sizes facilitate implementing progressive techniques like this.
Additionally, smaller schools allow closer student-faculty relationships. These mentoring relationships can guide students in mapping out individualized curricula to meet their needs. Faculty get to know each student’s strengths and areas for growth. This informs the types of learning experiences they recommend.
The intimate environment also builds community, which supports wellness and lifelong connections. Graduates become part of an extended network they can turn to throughout their careers as medicine evolves.
Envisioning the Future
While change can be challenging, rethinking traditional roles will position students for success. Just as precision medicine tailors treatments to individuals, precision education can customize learning. This strategy will equip graduates not just with current knowledge, but with the ability to adapt and stay at the forefront of medicine.
Medical education stands at an inflection point. Those schools that embrace emerging roles for teachers as mentors and students as partners will lead the way. They will produce physicians capable of thriving amidst the breakneck changes ahead.
At VTCSOM, their small size and supportive culture provides advantages as they build this innovative educational model. But all medical schools, both large and small, should reimagine teacher and student roles in light of the future needs of our healthcare system.
The pandemic provided a glimpse of how suddenly healthcare can be disrupted. We must prepare future clinicians not just for today’s challenges, but for the creativity and resilience to meet whatever comes next. That preparation starts with how we design medical education itself to be adaptable.
Dr. Harden has offered wise guidance rooted in decades of experience. Let us take up the call to collaborate in new ways to advance medical education. Our shared goal remains ensuring clinicians can deliver outstanding patient care, today and in the decades ahead.
Dr. Ronald Harden’s prediction that medical education must adapt to changing teacher and student roles provides an important wake-up call. His vision for partnership and precision education is prescient given the accelerating pace of change. By embracing this future now, innovative schools like VTCSOM can lead the way in developing clinicians equipped for lifelong learning. While challenging traditions is never easy, it is imperative we transform medical education to meet society’s needs. Our health and lives depend on graduating physicians prepared to tackle whatever the future holds.
Conclusion: Preparing Clinicians for the Future
From augmented diagnostics to robot-assisted procedures, AI will shape virtually every clinical practice. It is imperative that medical schools adapt quickly to prepare clinicians who can safely and effectively apply these emerging tools.
Updating curricula, pedagogies, learning environments, and mentorship opportunities will build students’ biomedical and digital literacy. It will produce a new generation of clinician-innovators who can ethically advance healthcare AI themselves. Educating medical students for the AI-enabled clinical environments ahead is critical to improving both health outcomes and healthcare delivery. By taking action today, medical schools can lead the way into a brighter technological future.

